HOW TO STOP PAIN IN ITS TRACKS: LOCAL/REGIONAL BLOCKS!
Tamara Grubb, DVM, PhD, CVMA, CVPP, Diplomate ACVAA
President, International Veterinary Academy of Pain Management (2023-2025)
Local anesthetic drugs are extremely effective, inexpensive and easy to use. When local anesthetic drugs are administered, pain impulses originating in the periphery are blocked and prevented from reaching the central nervous system. This blockade has several positive consequences:
The sensation of pain is alleviated or even eliminated for the duration of the block. Local anesthetic
drugs work by blocking sodium channels in nerve membranes so that the threshold potential is not
achieved and an action potential is not propagated, thus the pain impulse is not propagated. Local
anesthetics bind more readily to ‘open’ channels, thus rapidly firing nerves are more susceptible to
blockade.
- Analgesia allows the patient to be maintained under a lighter plane of anesthesia and this makes the anesthetic episode safer for the patient. In fact, local anesthetic drugs decrease the minimum alveolar concentration (MAC) of all anesthetic gases.
- The likelihood that ‘wind-up’ or hypersensitization will occur is greatly decreased because the portion of the pain pathway called ‘transmission’ is blocked. Transmission involves the conductance of pain impulses from the peripheral nociceptors to the dorsal horn neurons in the spinal cord. The neurons in the dorsal horn are responsible for central sensitization. By blocking input to these neurons, central sensitization (or ‘wind up’) is less likely to occur.
- And blocks are very cost effective!!
Commonly used local anesthetic drugs in veterinary medicine include
Lidocaine
- Onset of action: rapid; approximately 1-2 mins (less than 5 minutes)
- DOSE: 4-6 mg/kg in the dog and 2-4 mg/kg in the cat
- Duration of action: 60-120 minutes
- Convulsive dose in dogs: 11-20 mg/kg; Lethal dose in dogs: 16-28 mg/kg
- ‘Toxic dose’ in cats reported as 6-10 mg/kg
Bupivacaine
- Onset of action: approximately 5-10 minutes (up to 20 minutes)
- Duration of action: 4 to 6 hours
- DOSE: 1-2 mg/kg in the dog and 1 mg/kg in the cat
- Convulsive dose in dogs: 3.5-4.5 mg/kg IV
- Lethal dose in dogs: 5-11 mg/kg IV
- Data is mostly anecdotal in the cat but the general feeling is that 3 mg/kg IV is the toxic dose
- NOCITA®: (not available in all countries) liposome-encapsulated bupivacaine that provides
- analgesia for 72-hours.
- FDA-approved in both dogs (5.3 mg/kg) and cats (10.6 mg/kg)
- FDA-approved for tissue infiltration (dog) and peripheral nerve block (cat) but used for both tissue infiltration and nerve blocks in both species.
- Injection technique important – put the liposomes where you want them – ie, deliberate, thorough injection into the tissues/around the nerves.
Ropivacaine
- Onset of action: approximately 5-10 minutes (up to 20 minutes)
- Duration of action: 4 to 6 hours
- IMPORTANT POINT: Less cardiotoxic than bupivacaine
- DOSE: 1-3 mg/kg in the dog and 1-2 mg/kg in the cat
- International Veterinary Academy of Pain Management IVAPM.org
- Convulsive dose in dogs: 20 mg/kg IV
- Lethal dose in dogs: 42 mg/kg IV
- No data in cats but predicted to have same wider safety range than bupivacaine
Mepivacaine
- Onset of action: 2-5 minutes (up to 10 minutes)
- Duration of action: 2-3 hours
- DOSE: 3-5 mg/kg in the dog and 2-3 mg/kg in the cat
- Used primarily for diagnostics in equine lameness but effective for all blocks
- Lethal and convulsive dose in dogs: 29 mg/kg
- No toxic dose published for cat
Additions to local blocks to prolong duration of action (potentially up to 24 hrs), minimum dosages:
- Buprenorphine: 0.003–0.004 mg/kg (Snyder & Snyder, 2016; Grubb & Lobprise 2020)
- Dexmedetomidine: 0.0001 mg/kg (Bartel et al., 2016; Grubb & Lobprise 2020)
Adverse effects of local anesthetic drugs
Adverse events are extremely rare but can include any of the following:
- Local tissue effects – swelling, bleeding, inflammation, ‘tingling’? (unknown if this occurs in animals)
- Central nervous system – muscle tremors, seizure, coma
- At lower concentrations, depression of inhibitory neurons occurs and can cause cerebral excitation, which may lead to seizures. At higher concentrations, profound CNS depression with subsequent coma, respiratory arrest and death can occur. The latter is more likely following IV boluses of large doses.
- Cardiovascular system – the myocardial conduction system is sensitive to local anesthetics and IV boluses, especially of bupivacaine (but not NOCITA – high safety margin) can result in cardiovascular collapse. ONLY LIDOCAINE CAN BE ADMINISTERED IV.
- Anaphylaxis – rare, more common with esters (but still rare).
- Methemoglobinemia – rare, but can occur in cats.
Commonly used local anesthetic blocks in veterinary medicine (starting with the author’s favorite – and most commonly used - blocks)
For many of the blocks listed below, a suggested volume of drug is listed based on the amount of drug that can physically be injected into the site. However, with all blocks, the total dose that the patient can receive should be calculated and the cumulative dose (add up the dose or volume injected for each block) should not exceed this total dose.
- Advanced techniques: All of the blocks in this manuscript can be completed with appropriate knowledge of anatomy, good palpation skills, a needle and syringe. However, more advanced techniques (nerve locators, ultrasound guidance) can also be used and may be an option for some practices. Desensitization for some blocks (e.g., brachial plexus) may be more consistent with these techniques, whereas for some blocks (e.g., intraperitoneal lavage) these techniques are not useful.
A. General blocks
- ‘Field’ block (also called incisional block or line block)
- Blocking the ‘field’ of surgery. Local anesthetic drugs can be administered around the incision or directly into the incision. It is NOT true that lidocaine in an incision causes a delay in healing.
- NOCITA is a good choice for long duration ‘field’ block in both dogs and cats. Duration = 72 hrs.
- Indwelling catheter block (long duration field block)
- Indwelling, or ‘soaker’, catheters should be considered for large wounds or incisions that may be difficult to block or that may require continuous or intermittent delivery of drug for several days.
- The catheters can be buried in or near incisions and local anesthetic infused through the catheter to provide longer analgesia.
- Very useful for surgeries with large incisions, e.g.: amputations, mastectomies, etc.
- Local anesthetic drugs can be infused via a pump or administered by intermittent injection (eg, q 6–8-hour injections of bupivacaine at 1-2 mg/kg).
- The catheter is generally removed in 48-96 hours but can be left in longer.
B. Blocks on the Head
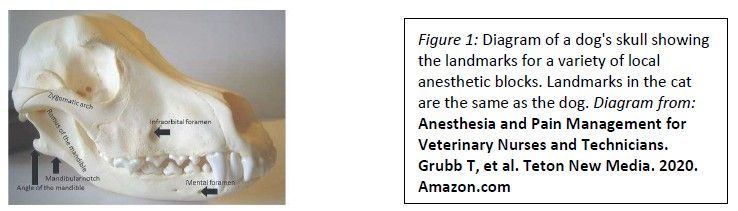
- Maxillo-facial (‘dental’ or ‘oral’) blocks (Figure 1)
Blocks listed below will cause unilateral desensitization from the site of injection rostrally to
midline.
- Maxillary or infraorbital nerve block – cranial approach
- The infraorbital nerve exits the infraorbital foramen, which can be palpated as a depression in the buccal mucosa dorsal to the root of the maxillary 3rd premolar (just cranial to the root of the 4th premolar or carnassial tooth in the area where the gingiva on the maxillary bone and the gingiva on the lip join).
- Block the nerve by injecting local anesthetic under the gingiva just rostral to the foramen or insert the tip of the needle into the infraorbital canal and inject. Injecting into the foramen insures more caudal spread of the block but is not necessary if the oral surgery site is rostral to the foramen. Also, the foramen can be difficult to locate or to enter in small dogs and cats & infusion rostral to the canal is still useful as there will be some caudal migration of the local anesthetic into the canal.
- A vessel runs with this nerve, so aspirate, then slowly infuse drug
- The volume that can be injected is approximately 0.1 to 1.0 ml, depending on patient size.
- Caudal Maxillary
- The caudal maxillary approach is often preferred over the infraorbital approach because the field of desensitization is much larger. This block will desensitize all ipsilateral tissue from the caudal molars rostrally and from the skin to midline. Use this approach if working on the caudal molars or doing surgeries on the nares, nasal passages, sinuses, soft palate or any other structures of the maxilla. In cats and brachycephalic dogs, the distance from the infraorbital foramen to the pterygopalatine fossa (where the maxillary nerve and its branches enter the skull) is very short and caudal diffusion of drug injected at the infraorbital foramen may be adequate for blocking the caudal structures of the skull.
- Extraoral approach 1 (extraoral, from zygomatic arch): Insert the needle percutaneously along the ventral border of the zygomatic arch approximately 0.5 cm caudal to the lateral canthus of the eye. The needle is kept horizontal and directed medially and slightly cranially (in an angle that would draw an imaginary line with the premolars on the opposite side of the head) until it hits bone. At this site, the maxillary nerve enters the pterygopalatine fossa.
- Extraoral approach 2 (extraoral, from bony orbit): Approach the pterygopalatine fossa from the bony orbit. The needle is placed at the midpoint of the ventral rim of the bony orbit and inserted straight down between the globe and the bone.
- Intraoral approach: Open the mouth as wide as possible. From inside the mouth, insert a short needle of no more than 2-4 mm (to avoid being close to the globe) inside the mouth just caudal and medial to the last molar.
- For all 3 techniques, aspirate and inject. The volume that can be injected is approximately 0.1 to 1.0 ml, depending on the patient’s size.
- Mandibular nerve block
- The mandibular foramen or the mandibular nerve can often be palpated on the lingual side of the mandible just rostral to the angle of the mandible and just caudal to the last molar in approximately the middle 1/3rd of the mandible (as measured from top to bottom).
- Regardless of whether the nerve or foramen can be palpated (often difficult to palpate in very small patients), the landmarks described above will be utilized for deposition of local anesthetic drug.
- The nerve ENTERS the mandible at the mandibular foramen and cannot be blocked between the mandibular foramen and the mental foramen.
- Intraoral technique:
- With the patient’s mouth supported in the open position (ie, use a mouth gag, roll of tape or some other method to ensure that the patient doesn’t close its mouth while your hand is in the oral cavity), direct the tip of the needle to the site described above.
- REMEMBER: Rigid mouth gags should NOT be used in cats. They can cause occlusion of the maxillary artery with resultant blindness and/or neurologic complications.
- Aspirate, then slowly infiltrate (0.2 -2.0 mls). The foramen cannot be entered so the drug is merely infused under the gingiva at the site of the nerve.
- Extraoral technique:
- Landmarks are the same as those described above but the approach is from the outside, through the skin at the angle of the mandible. This technique is easier than the intraoral technique in cats and in some small dogs.
- Pass the needle through the skin along the medial aspect of the mandible to a point where the tip of the needle is at the site of the foramen (again, aiming for a site just caudal to the last molar on the lingual side of the mandible).
- With a finger in the oral cavity the needle can be felt under the gingiva.
- When the site near the mandibular foramen is reached, aspirate and inject the local anesthetic drug (0.2-2.0 mls).
- Mental nerve block
- The mandibular nerve EXITS the mandible at the middle mental foramen which can be palpated just ventral to the root of the 2nd premolar, immediately caudal to the labial frenulum.
- Insert the needle tip just cranial to the foramen, aspirate and slowly infuse 0.1-0.5 mls local anesthetic. Apply digital pressure over injection site for 30-60 seconds to ensure maximum caudal/distal diffusion of the drug into mandibular canal.
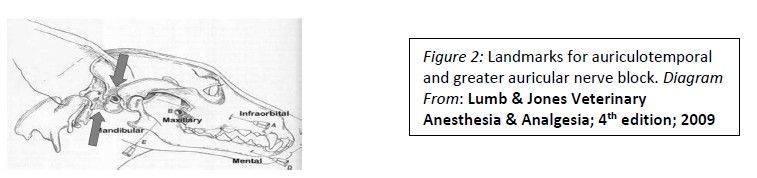
- Auriculotemporal and greater auricular nerve block (Figure 2)
- Blockade of these nerves will desensitize the inner surface of the auricular cartilage and the external ear canal
- Insert 23 ga. 1-1 ½ inch needle subcutaneously rostral to the vertical ear canal and directed towards the base of the ‘V’ formed by the caudal aspect of the zygomatic arch and the vertical ear canal
- Insert the same sized needle subcutaneously ventral to the wing of the atlas and caudal to the vertical ear canal and directed parallel to the vertical ear canal
- Inject 0.5-1.5 ml (depending on size of dog) at each location
C. Blocks of the thorax, abdomen and genital-urinary system
- Testicular block (Figure 3)
- Insert the needle into the body of the testicle with the tip pointed towards the body of the patient. ASPIRATE.
- Inject lidocaine or bupivacaine into the body of the testicle until you feel ‘pressure’ or until the ‘dose’ (see below) has been injected
- The drug will migrate up the spermatic cord.
- The dose will be volume limited due to the size of the testicular tissue
- Calculate 1 mg/kg bupivacaine or 4 mg/kg lidocaine and the volume that will ‘fit’ is about ½ of the calculated volume
- This will generally be 0.2-2.0 ml per testicle in dogs and cats
- For an incision directly over the testicle (cats), continue infiltrating as the needle exits the testicular body to block the skin and subcutaneous tissue.
- For an incision in another location (dogs), inject local anesthetic in skin and subcutaneous tissue at the incision site.

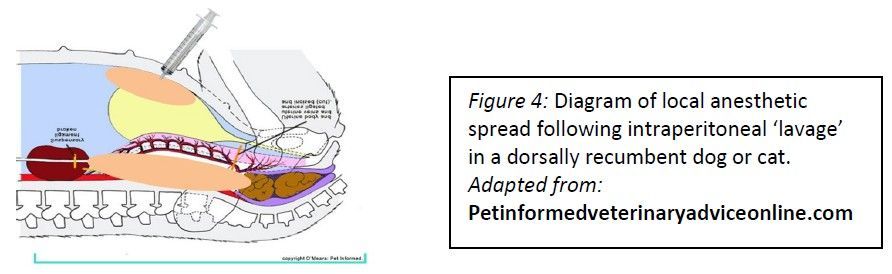
- Mesovarium block or peritoneal lavage (Figure 4)
- The mesovarium can be infiltrated with lidocaine.
- The volume will be about 0.5 mls per side in small dog or cat and up to 3.0 mls/side in large dog.
- Elevate either ovary, infiltrate mesovarium, elevate opposite ovary, infiltrate mesovarium, remove first ovary, remove the second ovary and proceed with the ovariohysterectomy.
- My favorite: the peritoneal cavity can be ‘bathed’ or ‘lavaged’ with local anesthetic.
- After opening the linea (preferred) OR after completing the OHE, draw up 2-4 (cat) – 4-6 (dog) mg/kg lidocaine OR 1-2 (cat) – 2-4 (dog) mg/kg bupivacaine and, if necessary, dilute the drug with saline – the total volume needs to be 0.4-0.6 ml/kg to ‘lavage’ or ‘bathe’ the entire abdominal cavity. ‘Bathe’ the peritoneal cavity with the mixture by instilling it into the abdomen through the incision. Complete the OHE and close the incision as usual.
- This technique may be more effective than mesovarium block since analgesia will be provided at both the ovarian and uterine surgical sites.
- Publications are available in both dogs and cats for the efficacy of this block for OHE. In humans, the block is also used for abdominal exploratory surgeries and cesarean sections. These uses are also common in veterinary medicine, but there are no research studies.
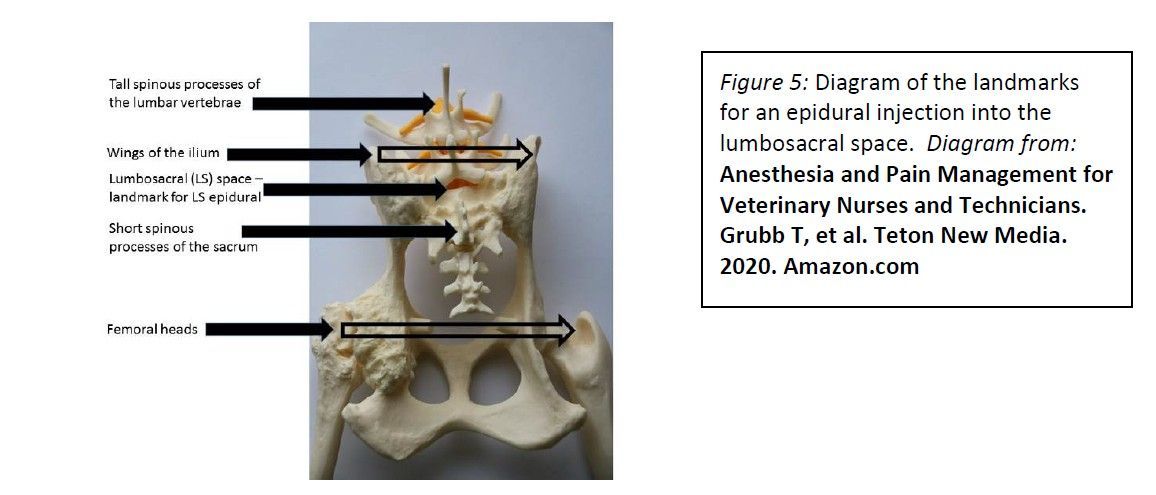
- Lumbosacral epidural analgesia (Figure 5)
- Opioids are most commonly used but local anesthetic drugs can be used in conjunction with opioids.
- 0.1 mg/kg morphine (preservative-free is gold standard but morphine with preservative is commonly used in veterinary medicine)
- Dilute to 1 ml/4.5 kg with bupivacaine, sterile saline or sterile water
- Provides up to 24 hours of analgesia with little to no systemic effects. The opioids will cause sensory blockade but will not cause motor blockade. The local anesthetics can cause motor blockade, however, the motor effects are generally minimal or absent by the time the patient recovers from anesthesia to the point that it is ambulatory.
- Consider for any pain in caudal half of patient. Examples include, rear limb soft tissue or orthopedic surgery, abdominal exploratory and bladder surgeries, surgeries on the tail or perineal region, etc.
- Technique:
- Place the anesthetized patient in sternal or lateral recumbency
- Legs can be placed forward or to the back. I prefer forward in cats and small dogs.
- Locate the wings of the ilium and palpate the lumbo-sacral (LS) space (almost directly in line with the wings of the ilium on the mid-line).
- Clip and scrub this region. Wear gloves and use a small drape or glove wrapper.
- Insert an epidural needle into the caudal portion of the LS site with the needle angled at approximately 45o from vertical.
- Slowly advance the needle until the epidural space is entered.
- ‘Hanging’ drop often works (aspiration of fluid in the hub of the needle as the epidural space is entered).
- Several ‘pops’ will be felt.
- ‘Walking off’ the bone is the most definitive determination of proper placement of the needle in between vertebrae.
- STOP as soon as the space is entered and slowly inject the drug.
- The drug should inject easily if the needle is in a space.
- Stop injecting and take your thumb off the plunger. the fluid should momentarily continue to flow if the tip of the needle is in the epidural space. This is the most definitive determination that the needle is in the lumbosacral space.
- If the drug does not inject easily, back up a VERY tiny amount and try again.
- Once the drug has been injected, remove the needle and proceed with surgery.
- If local anesthetic drugs have been used, may want to lay patient with surgical side down for about 5 minutes.
- Opioid epidurals do NOT affect motor function of the rear limb or diaphragm. Local anesthetic drugs can affect motor function but rarely do (volumes that are described here do not migrate far enough cranially to affect the diaphragm so ventilation is not impaired).
- Complications include ineffective or incomplete block (by far the most common complication), epidural hematoma or abscess, hyperalgesia (VERY rare). Contraindications include bleeding disorders (to prevent hematomas) and skin disease over the LS space (to prevent abscesses).
- Abnormal pelvic anatomy (either from congenital lesions or trauma) may make epidurals difficult.
- Epidural catheters are fairly easily placed in larger dogs and can be maintained for several days to allow continuous or intermittent delivery of analgesic drugs.
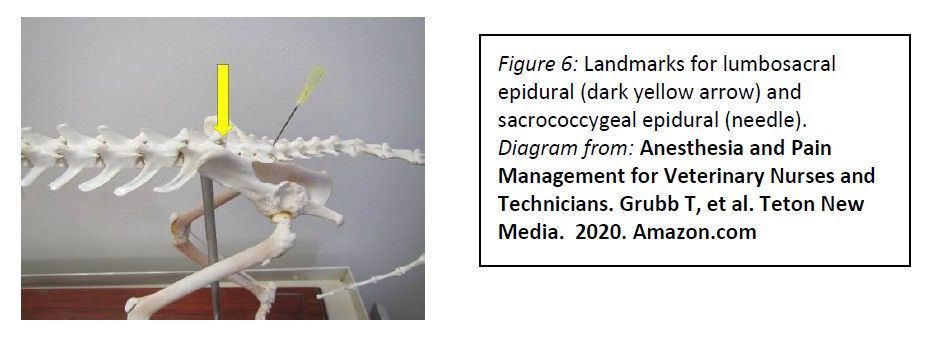
- Sacrococcygeal or intercoccygeal epidural (Figure 6)
- This block is often used to provide analgesia for tail amputations, perineal urethrostomies, and placement of urinary bladder catheters for urethral obstructions.
- Move the tail up and down in a ‘pumping’ motion while palpating the sacrococcygeal region of the patient. The first movable space at the caudal end of the sacrum is either the sacrococcygeal or intercoccygeal space. Either site is appropriate for injection.
- Insert a 22-G needle through the skin ON MIDLINE at a 45-degree angle to the skin surface.
- Proceed slowly until needle enters the space (generally hit bone and ‘walk off’ the bone).
- Hanging drop technique often works. Should have no resistance on injection.
- Use lidocaine for rapid onset (0.1-0.2 ml/kg 2% lidocaine), can add an opioid (same as for lumbosacral epidural) for long-term analgesia. Don’t inject air, air bubble may cause incomplete block since this is a very small space.
- Intercostal block
- Inject local anesthetic in the tissues caudal to the proximal portion of the ribs. Inject local anesthetic in 2-3 rib spaces in front of and 2-3 rib spaces behind the area that needs to be desensitized.
D. Blocks of the limbs
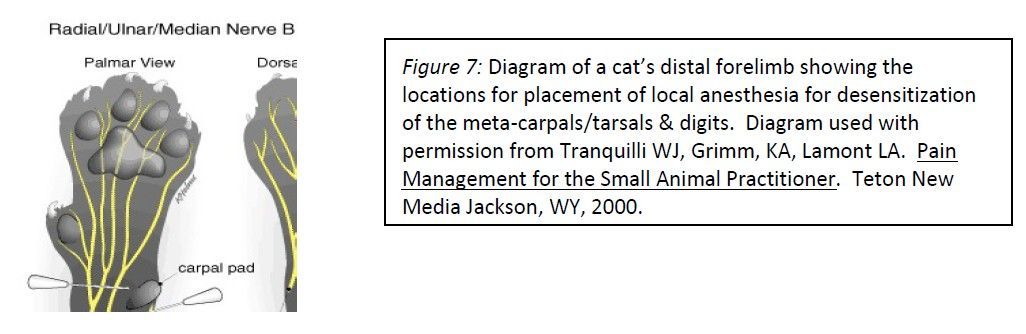
- Metacarpals/metatarsals/digits block (Figure 7)
- Four different ways to block
- Three point (or four point)
- Locate the carpus and the accessory carpal pad
- Inject 0.1-0.3 mls subcutaneously at three sites:
- 1) medial to the accessory carpal pad (blocks median nerve and palmar branch of the ulnar nerve);
- 2) lateral and proximal to the accessory carpal pad (blocks dorsal branch of the ulnar nerve); and
- 3) on the dorsal-medial portion of the carpus (blocks superficial branches of the radial nerve).
- NOCITA FDA-approval in cats is for a similar (4-point) block.
- Ring block
- Similar to three-point block but use a subcutaneous ‘line’ of local anesthetic all the way across the dorsum of the paw and another ‘line’ all the way across the ventrum of the paw just above the location of the accessory carpal pad to provide a ‘ring’ of local anesthesia that desensitizes the nerves described above.
- Interdigit or ‘digital’ block
- Block between each toe
- ‘Splash block’
- ‘Splash’ local anesthetic into incision
- Not as effective as other methods
- Brachial plexus block
- Locate the point of the shoulder, the first rib and the transverse processes of the cervical vertebrae.
- Insert a 2-3-inch needle (an epidural needle will work) at the point of the shoulder to the point where the tip of the needle is even with the first rib. Keep the needle horizontal during placement so that the tip does not enter the thoracic cavity.
- Aspirate, then inject 1/3 of the local anesthetic (1 (cat) or 2 (dog) mg/kg bupivacaine diluted with saline to a total 1 ml solution per 4.5 kg body weight) at this site, slowly withdraw the needle to the middle of the area to be blocked, aspirate and inject 1/3 of the local anesthetic. Withdraw the needle to a site just before it exits the skin, aspirate and inject the remaining 1/3 of the local anesthetic.
- Intra-articular block
Inject 1-5 ml local anesthetic into the joint prior to surgery and repeat the injection after the joint has been sutured closed.
- If local anesthetics are concerning, use opioids! There are opioid receptors in the synovium and they are upregulated in inflammation. This seems like the joint’s way of screaming, ‘give me opioids!
- For chronic pain, steroids and specific products like radioactive tin and collagen ‘replacers’ may be injected.
E. Other uses of local anesthetic drugs
- Lidocaine constant rate infusions are effective and safe in a large variety of patients. Somewhat controversial in cats.
- Lidocaine patches have been used over incisions or painful cutaneous lesions in veterinary patients. In humans, lidocaine patches are used for deeper muscle pain and they may be effective for this type of pain in our patients too. But our patients would likely have to be shaved to get patch contact with the skin and this isn’t usually practical.
- There are a variety of creams & gels that may or may not work. Some of the local anesthetic creams work on the skin if they are placed on the skin and covered with a bandage for 30-45 minutes. These can be used to desensitize the skin for IV catheter placement. Lidocaine gel (you can make your own by just mixing some lidocaine into sterile lubricant) is an excellent lubricant for passing a urinary catheter.
References/Reading:
- Campoy L, Read M. Small Animal Regional Anesthesia and Analgesia. Wiley-Blackwell, 2013.
- Gruen ME, Lascelles BDX, Colleran E, Gottlieg A, Johnson J, Lotsikas P, Marcellin-Little D, Wright B. 2022 AAHA Pain Management Guidelines for Dogs and Cats. J Am Anim Hosp Assoc 2022; 58:55–76. https://www.aaha.org/globalassets/02-guidelines/2022-pain-management/resources/2022-aaha-painmanagement-guidelines-for-dog-and-cats_updated_060622.pdf
- Grubb TL, Albi M, Ensign S, Holden J, Meyer S, Valdez N. Anesthesia and pain management for veterinary nurses and technicians. Teton New Media, WY, 2002. https://www.amazon.com/Anesthesia-Management-Veterinary-Nurses Technicians/dp/1591610508/ref=sr_1_2crid=1K8V5UOBIYU1J&keywords=Grubb+book+veterinary&qid=1645837731&sprefix=grubb+book+veterinary%2Caps%2C171&sr=8-2
- Grubb T, Lobprise H. Local and regional anaesthesia in dogs and cats: Overview of concepts and drugs (Part 1). Vet Med Sci. 2020 May;6(2):209-217. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7196681/
- Grubb T, Lobprise H. Local and regional anaesthesia in dogs and cats: Descriptions of specific local and regional techniques (Part 2). Vet Med Sci. 2020 May;6(2):218-234. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7196680/
- Lerche P., Aarnes T.K., Covey-Crump G., Martinez Taboada F. (2016) Handbook of Small Animal Regional Anaesthesia and Analgesia Technique, Wiley Blackwell, Hoboken, N.J.
- Monteiro BP, Lascelles BDX, Murrell J, Robertson S, Steagall PVM, Wright B. 2022 WSAVA guidelines for the recognition, assessment and treatment of pain. J Small Ani Pract 2022;64 (4):177-254. https://onlinelibrary.wiley.com/doi/10.1111/jsap.13566
- Otero P, Portela DA. (2018). Manual of small animal regional anesthesia: Illustrated anatomy for nerve stimulation and ultrasound-guided nerve blocks. https://www.researchgate.net/publication/327663189_Manual_of_small_animal_regional_anesthesia_Illustrated_anatomy_for_nerve_stimulation_and_ultrasound-guided_nerve_blocks
- Steagall PVM, Benito J, Monteiro B, Lascelles D, Kronen PW, Murrell JC, Robertson S, Wright B, Yamashita K. Intraperitoneal and incisional analgesia in small animals: simple, cost-effective techniques. 2020;1(1):19-23. https://onlinelibrary.wiley.com/doi/10.1111/jsap.13084
- Videos: Go to WSAVA.org; go to tab ‘committees’, click on ‘global pain council’, scroll down to ‘Pain Management Guidelines’ (manuscript) and ‘Educational Videos’ (local block videos!). https://wsava.org/committees/global-pain-council/







